Key points you should know:
- The NIH made key structural errors in setting up RECOVER, namely concentrating funding with a small number of researchers and, in selecting those researchers, failing to prioritize people who had experience in studying or treating post-infectious chronic diseases before the pandemic.
- Structural issues with RECOVER fit into broader patterns with the NIH’s process for awarding grants, experts said, including the agency’s tendency to fund the same researchers and institutions multiple times and a historical lack of funding for large-scale projects about post-infectious chronic diseases.
- RECOVER has failed to meet its stated goals of defining long COVID, tracking incidence and prevalence, finding novel treatments, and prioritizing patient input. While patient representatives’ experiences vary and the program has improved its engagement processes in the last two years, representatives who spoke with The Sick Times said that their feedback has not been as central to research directions as the program’s initial goals suggest.
- Recent decisions made around the clinical trials, such as the continuation of trials examining exercise and pacing despite pushback from outside researchers and advocates, suggest that RECOVER may be unable to learn from its early issues to the extent needed to regain community trust, some experts say.
- While some researchers and patient advocates say RECOVER can still provide valuable insight into Long Covid, others suggest this program, and perhaps even the NIH as a whole, should not be a priority for future long COVID funding from the federal government. Researchers and advocates recommend other federal agencies and offices that may be more suited to innovation, particularly in quickly running clinical trials.
In February 2021, the National Institutes of Health (NIH) launched a new $1 billion initiative to study long COVID, a chronic disease that has changed the lives of millions of Americans. Then-NIH director Francis Collins laid out the program’s goals in a blog post: find the biological causes of long COVID, determine how many people are impacted, and identify treatments.
Three years later, the NIH initiative, called RECOVER, has not met these goals, according to a detailed review of budget and planning documents obtained through the Freedom of Information Act and shared with long COVID experts. RECOVER’s research into long COVID’s underlying biology has lagged behind that of privately-funded scientists; it has failed to provide reliable estimates of how many people have long COVID; and clinical trials, launched last summer, garnered extensive criticism for failing to test promising treatments.
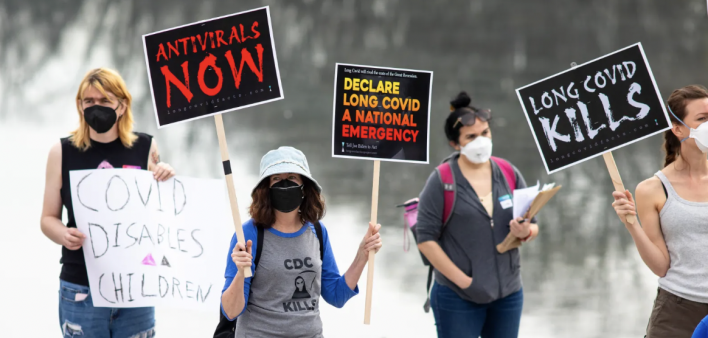
As RECOVER approaches the end of its initial $1.15 billion, four-year funding allocation, people in the long COVID community are questioning whether future funding — including an additional $515 million allocated this year — would help the initiative turn around or would lead to more slow, minimal progress. Many researchers and clinicians outside the program and people with long COVID have lost faith in RECOVER’s ability to deliver meaningful answers about this complex disease. Some have lost faith in the NIH entirely.
“We gave [the NIH] a chance and they bungled it,” said John Bolecek, who has lived with long COVID for two years and closely followed RECOVER. The program has done nothing “to narrow down what’s actually going wrong with people,” or identify treatments, he said. Like other researchers and advocates, Bolecek would like to see future funding go to federal agencies that can support faster, more innovative trials, such as the Department of Defense.
New records from the NIH, shared with The Sick Times, MuckRock, and STAT News in response to a FOIA request, provide new insights into how RECOVER failed to deliver on its initial goals. The records include applications that the three initial core institutions of RECOVER — New York University, Massachusetts General Hospital, and Research Triangle Institute — sent in response to the NIH’s initial solicitation for grant proposals in early 2021 and contracts between the NIH and these three institutions.
Combined, the three contracts represent about $934 million of the total $1.15 billion that Congress allocated to the NIH for long COVID research in 2020. The documents reveal how the agency set up its flagship long COVID research initiative, including the scientific expertise that NIH reviewers prioritized in selecting research teams to lead RECOVER and the early goals and timelines of the program.
One foundational problem is that the NIH did not select scientists with “an established background in conducting research on post-acute infection syndromes” to lead the initiative, said David Putrino, Nash Family Director of the Cohen Center for Recovery from Complex Chronic Illness at Mount Sinai, who reviewed the documents. More recent decisions by RECOVER’s leadership, such as the treatments selected for clinical trials, demonstrate how this lack of expertise and understanding of long COVID’s complexity has permeated through the program, Putrino and other experts said.
RECOVER’s failure to meet its goals follows a history of the NIH failing to support innovative research into these complex diseases, Putrino said. He has told NIH leaders that they should take responsibility for the lack of progress and “apologize to the American people” to reestablish faith in the program, he said.
“I completely understand why [the long COVID community] is frustrated, I completely understand why they think we’re being slow,” said NIH Director Monica Bertagnolli in an interview. She said RECOVER’s pace was necessary to understand key aspects of long COVID, learn from patients and set up trials that will produce accurate results. “The infrastructure is now there,” she added, “And we are, with urgency, going to charge ahead as best we can.”
Further information from the NIH, sent in written responses to questions, defended many decisions made in RECOVER, including its selection of research teams to lead the program, inclusion of patient advocates in advisory groups, upcoming scientific publications, and choices about clinical trials.

Chart: Betsy Ladyzhets. Source: National Institutes of Health. Created with Datawrapper
NIH selected teams without relevant expertise
The application materials demonstrate that the research teams put in charge of RECOVER were not qualified to lead this foundational long COVID inquiry, according to outside scientists and patient-advocates who reviewed the documents. In their applications, dozens of scientists from NYU and Mass. General shared details from their research backgrounds that they believed were most relevant to the program; none mentioned the post-infectious chronic diseases that predate the COVID-19 pandemic and are now commonly diagnosed alongside long COVID.
Researchers who spent their careers studying these diseases — such as myalgic encephalomyelitis (ME), postural orthostatic tachycardia syndrome (POTS), and mast cell activation syndrome (MCAS) — before 2020 were poised to use their expertise for long COVID, scientists and patient-advocates agreed. The ME community, in particular, anticipated in early 2020 that some people infected with the coronavirus would later develop chronic disease.
Yet the NIH did not tap these experts to lead RECOVER. The teams selected “did not have experience in this arena before the pandemic,” said Jaime Seltzer, scientific director of #MEAction. This lack of experience “dramatically and demonstrably” impacted how they designed the research as well as their interactions with the long COVID community, she said.
Instead, the NIH selected for leadership, as Putrino put it, “a bunch of biostatisticians and epidemiologists.” In their applications, the research teams highlighted experience with collecting and utilizing electronic health records, clinical test results, genomics, and other types of health data to answer biomedical questions. This focus aligns with a broader agency-level interest in “big data” under former director Francis Collins, said Stephen Smith, a patient-advocate who closely follows research and runs the Twitter/X account Post-Viral Trials News.
A “big data” approach is challenging for diseases like long COVID because these syndromes are so complex and not described well by current medical technologies, Smith said. Standard medical tests and diagnostic codes often don’t capture the myriad of symptoms that patients experience.
Without experience in the symptoms and biological abnormalities that characterize post-infectious diseases, the RECOVER researchers weren’t prepared to collect data that would accurately describe long COVID, Smith said. The researchers were faced with “garbage data in, garbage data out,” he said.
The NIH selected teams to lead RECOVER “based on a range of research expertise and the scientific merit of their proposals,” the agency said in a statement. Scientists and clinicians with expertise in post-infectious chronic diseases “informed the RECOVER Initiative design and continue to be involved” in different committees, the NIH said, sharing a list of involved experts. All but two of these experts are not part of RECOVER’s publicly-listed leadership, however, and one, Leonard Jason at DePaul University, told The Sick Times that he is no longer part of RECOVER after the advisory committee in which he participated was discontinued last year.
Leora Horwitz, a principal investigator for the RECOVER adult observational study at NYU, became interested in the project due to her experience caring for COVID-19 patients in spring 2020 and her research at the Center for Healthcare Innovation and Delivery Science, which focuses on “using our own data to understand healthcare better,” she told The Sick Times. She and her colleagues started studying long COVID by tracking those early patients after they were discharged from the hospital, which informed their application to RECOVER, she said.
Horwitz acknowledged that long COVID can be tough to track through electronic health records, pointing to complex symptoms such as post-exertional malaise that are not recognized by many doctors. RECOVER’s observational arm has addressed this challenge by asking patients directly about their symptoms and improving those surveys over time based on participants’ feedback, she said. For example, the adult study has added more questions about ME and MCAS over time.
The NIH’s failure to select a qualified team to lead RECOVER is part of a broader pattern of issues with the agency’s grant review process, Smith, Putrino, and other experts said. Unlike other agencies and research institutions that have adopted anonymity into their grant review process, the NIH continues to heavily weigh where researchers work and their prior records of NIH support.
As a result, the NIH tends to award funding to researchers and institutions who have previously received NIH funding, creating an insular cycle that discourages unique innovation. One 2022 analysis of this problem, by the research nonprofit New Science, found that just ten universities receive 22% of the NIH’s extramural grant budget. Report author Matt Faherty described the agency as “risk-averse” and warned that it is “missing out on ambitious, transformative ideas” across fields.
This pattern creates a particular challenge for researchers of post-infectious diseases like long COVID because the NIH has historically not funded large, ambitious research projects in this field. As a result, when the pandemic started, there weren’t research teams who had both the right disease expertise and the success in running large, multi-site studies that the NIH sought for RECOVER, said ME researcher and advocate Mary Dimmock.
Bertagnolli acknowledged this challenge, saying that past ME research has been smaller in scale and has not answered key questions about that disease.
The agency may have been more successful in supporting long COVID advancements if it had used the $1.15 billion over many smaller initiatives, rather than dumping the entire allocation into RECOVER, Dimmock suggested. “All the money that they have is tied up in this one initiative, which means a lot of the people who could be conducting research are not getting any opportunity to do so,” she said.
Failure to meet goals, listen to patient expertise
The documents also share novel details about RECOVER’s original goals and proposed timelines, many of which have still not been met three years into the initiative. One of those original goals was to better define long COVID and identify how many people in the U.S. are living with the disease as well as the risk of developing it after a coronavirus infection. Despite receiving significant funding, the initiative’s observational study has not produced these estimates.
Some experts attribute this lack of data to poor recruitment, particularly of control participants who could be compared against those with long COVID. According to the NIH’s contract with NYU, the observational study was set to have recruited 85% of its cohort by the end of its first year, in spring 2022, and to have a “working research-based definition” of long COVID in the same timeframe.
Yet the study had not met either goal by April 2023, according to prior reporting by MuckRock and STAT News. While RECOVER quickly met enrollment goals for people who already had long COVID symptoms, it was still looking for control participants as of that time. The program lost its opportunity to recruit such participants before the vast majority of Americans were infected during Omicron waves, Smith said: the program “had the resources to come up with good prevalence and incidence numbers, and they didn’t.”
When asked about recruitment, Horwitz said that filling the control spots in RECOVER extended the recruitment period, as did meeting the observational study’s goals for diversity. “We took very seriously our mandate to look like America,” she said, describing efforts to recruit participants who were Hispanic, didn’t speak English, and lived in rural areas. The resulting cohort provides a unique opportunity for long-term research, she said, as it includes thousands of people who have been closely tracked from their first COVID-19 infections.
RECOVER did share a working definition of long COVID in May 2023, with a paper published in the Journal of the American Medical Association. However, the paper quickly garnered criticism from the long COVID community, as patient-advocates and researchers questioned the symptoms it prioritized for diagnosis. One letter by the advocacy group Long COVID Action Project asking the NIH to consider corrections and retraction was sent thousands of times to officials and study authors. “RECOVER posted a Q&A in response to concerns,” the NIH said. Acknowledging the criticism, Horwitz said that the paper affirmed a long COVID diagnosis for many people and “helped to convince the medical community that this is a legitimate syndrome.”
To Horwitz, the key goal of the observational research is to identify “what long COVID looks like,” including prominent symptoms, potential subtypes, and paths for recovery, as this information provides benchmarks for clinical trials, she said. NYU’s application and contract with the NIH similarly establish that observational research was considered necessary before clinical trials could begin. Outside scientists, however, question this allocation of resources given the extensive research going on outside RECOVER that has already provided many answers.
The definition paper is one of about 50 that RECOVER researchers have published so far. Matching the program’s focus on “big data,” the majority of these studies use electronic health records or data from the observational cohorts rather than presenting novel information about the underlying biology of long COVID. About 100 additional papers are in the process of development and peer-review, according to the NIH, but it’s difficult to estimate when they will be made public due to the slow progress of scientific publishing.
Most public progress on identifying long COVID’s causes so far has come from privately-funded research, scientists and patient-advocates say. This could shift if RECOVER follows another one of its original goals: making its data and biospecimens available to other researchers. The NIH announced last month that researchers could apply to analyze data from the observational studies; in the future, researchers will also be able to apply to access specimens collected for a biobank housed by the Mayo Clinic, the NIH said in its statement.
Another original goal of RECOVER, as outlined in the applications and contracts, was that researchers would engage with long COVID patients as a central facet of the program. One section of NYU’s application describes how the team planned to develop and support both national and local “patient engagement working groups” that would “identify key patient-centered factors” to include in each stage of research. The plan included several avenues for feedback, such as a “call center for participants with urgent questions.”
Patient representatives who spoke to The Sick Times and MuckRock said that their experience does not live up to this goal. According to the NIH, 59 patient representatives are involved with RECOVER as members of its advisory committees, along with 43 other caregiver, advocacy, and community representatives. Representatives describe varied experiences depending on which part of the programs they serve. But overall, patients are not leading research directions to the degree outlined by NYU’s proposal, representatives who reviewed the document said.
Four representatives who served on advisory committees for RECOVER’s clinical trials said that their feedback about trial interventions and study designs was dismissed by other committee members and the trials’ investigators. Patient representatives are “there to check a box, they are not seen as experts,” one of the representatives said.
These concerns are not new. In November 2021, the Patient-Led Research Collaborative (PLRC)*, a nonprofit research organization run by people with long COVID, organized an open letter to RECOVER leadership — signed by about 50 other research and advocacy organizations — that claimed patient engagement was “tokenizing and inadequate.” RECOVER addressed some of the letter’s concerns, such as creating a national group for all patient representatives to meet. But a lack of meaningful patient engagement at early stages of the program, as well as a lack of expertise in post-infectious chronic diseases, contributed to current problems with study design, said PLRC co-founder Lisa McCorkell. “Patient engagement was still forming” at the time of that letter, the NIH said.
Challenges with patient engagement reflect other organizational issues within RECOVER, such as a lack of clarity on who is responsible for decisions. Cindy Throop, a researcher and consultant who briefly worked for RECOVER as an analyst at Research Triangle International, described the program as “chaotic” in comparison to other contracts she’d worked on in two decades of experience with federal health agencies. “It was really unclear who was in charge,” she recalled, between the different academic institutions and NIH offices involved.
Throop, as well as patient representatives who have worked on RECOVER, also expressed surprise and confusion at being asked to sign a non-disclosure agreement for her participation. She had never been asked to sign such a document for a government contract, she said. “I never signed it,” she said, “and it was so chaotic, no one ever realized that I did not sign it.”
Clinical trials show lack of adaptation
Despite a mandate from Congress for the NIH to identify treatments for long COVID, clinical trials run by RECOVER have moved slowly and been fraught with criticism. Recent developments with these trials show that RECOVER has failed to address its organizational issues or build on long COVID research conducted outside the program, scientists and advocates say.
When clinical trials were announced last summer by RECOVER and the Duke Clinical Research Institute, which is coordinating this part of the program, experts and advocates characterized them as “underwhelming.” Rather than testing drugs that address the root causes of the disease, RECOVER’s trials test behavioral interventions and widely-available medications that many patients have tried already and found unhelpful for alleviating their symptoms. Experts also expressed concern about some aspects of the study’s designs, warning that the trials may fail to identify potential safety issues or determine whether treatments are effective.
The central example for this criticism is RECOVER-ENERGIZE, a pair of trials that launched this month. The trials aim to address patients’ challenges with exercise and other forms of exertion, which are common long COVID symptoms.
When ENERGIZE was first developed, experts and advocates warned that the trial could potentially harm patients by testing exercise as a treatment for long COVID. Many patients experience a symptom called post-exertional malaise (PEM), in which physical or mental exertion leads to debilitating fatigue and increased health issues, caused by dysfunction in how patients’ bodies produce and use energy. Clinical guidelines for long COVID and ME recommend against exercise for people who have PEM based on past research and patient experiences.
In response to these criticisms, the RECOVER team adjusted ENERGIZE’s study design to reduce the risk of harm. The researchers split the study into two trials, one testing an exercise regimen and the other testing pacing, a strategy for managing PEM. People who experience PEM will qualify for the pacing trial while only those without the symptom should be included in the exercise test, according to the study protocols. Lucinda Bateman, a clinician at the Bateman Horne Center who specializes in ME and long COVID, helped design the revised pacing trial.
Outside experts acknowledge that a pacing trial could have some value in demonstrating this strategy’s effectiveness for managing PEM. However: “I have so little faith in RECOVER at this point that I am much more worried that the study design will not be adequate to demonstrate that,” Seltzer said. For example, it’s unclear based on public information about the study how researchers will identify if someone in the exercise trial begins to experience PEM and should stop exercising, which could be a safety issue for participants, she said.
Even if RECOVER-ENERGIZE is successful, it’s not likely to “move the needle” on long COVID treatments, Putrino said, as pacing is a well-understood strategy that helps to manage symptoms rather than a drug that addresses their underlying causes. Like other researchers and patient-advocates, he would like to see the program stop this trial and instead use the funds for more promising treatments.
When asked why RECOVER-ENERGIZE is still moving forward, the NIH said, “it is critical to generate high-quality evidence” about rehabilitation approaches for fatigue and exercise intolerance, suggesting that prior studies have been small and not randomized controlled trials. “Study protocols were developed with input from patient representatives, advocacy groups, and scientific experts,” the NIH said.
Bertagnolli similarly emphasized the need for high-quality studies, saying that the “first wave” of RECOVER’s trials aim to provide “definitive answers” about treatments that have preliminary evidence behind them already, while a coming “second wave” may test more novel options.
RECOVER-SLEEP, another set of trials also launching this spring, has garnered similar criticism for testing basic interventions to improve sleep, like melatonin and light therapy, that are unlikely to make significant differences for patients. These trials are “really disappointing,” said Jon Douglas, a long COVID patient-advocate who has closely followed RECOVER.
The clinical trials, like other parts of RECOVER, are not led by researchers with backgrounds in post-infectious diseases, sources involved with advising trial development told The Sick Times and MuckRock. Patient representatives described meetings in which researchers were unfamiliar with basic tools of this field, such as autonomic testing.
In one public-facing example of this lack of expertise, patient-advocates and researchers point to a podcast interview with Adrian Hernandez, executive director of the Duke Clinical Research Institute, which is coordinating the RECOVER trials. Hernandez’s discussion of long COVID on this podcast suggests that he hasn’t learned from past research into ME, POTS, and related diseases, Smith said.
The long COVID community’s disappointment in RECOVER’s trials is leading to challenges with recruiting people into those studies, one patient representative told The Sick Times and MuckRock. Another barrier to recruitment is that people with the most severe long COVID symptoms are unable to enroll in the trials, as they require in-person visits to RECOVER sites. Katie Klocksin, one patient who inquired about enrolling in the program’s autonomic trials, was unable to participate due to the in-person requirements, she shared in an email.
Long COVID researchers and patient-advocates outside RECOVER emphasize that there are many other, more promising treatments that the program could be testing. For example, PLRC has compiled a long list including antivirals, drugs targeting the immune system, heart and gastrointestinal medications, and other drugs that could be repurposed from other diseases for long COVID. The list overlaps with drugs recommended by one of the NIH’s own leading ME researchers, Avindra Nath, said PLRC co-founder Hannah Davis.
In discussing RECOVER’s clinical trials, the NIH and Duke team has previously said these trials will use an “adaptive” platform that can quickly take out less promising treatments and add new options. Yet the researchers have not used this platform to its potential, experts and advocates say, as RECOVER has failed to pull treatments that would waste funding.
Can the NIH regain trust?
Disappointed in RECOVER’s slow progress, lack of novel research, and underwhelming clinical trials, many people in the long COVID community have lost faith in the program. While some advocates and researchers say the program could be turned around or adapted to a more efficient structure using the additional $515 million that the NIH provided in early 2024, others call for future funding to go elsewhere. This future funding could come from Congressional appropriations processes and a new bill proposed by Senator Bernie Sanders.
Experts and advocates acknowledge that there are some valuable parts of RECOVER that should continue, such as pathobiology studies with samples collected from patients in the observational study. Nita Jain, a biotech founder and patient representative working on upcoming scientific papers with RECOVER, thinks more in-depth examination of these samples could help answer questions about changes to the immune system and other biological changes that occur in long COVID.
Research on these samples, stored in a biobank at the Mayo Clinic, has been limited so far, Jain said. She hopes additional funding can support such molecular biology work as well as research by private companies. “Cautiously optimistic is my state of mind right now,” she said of RECOVER’s future.
RECOVER also provides an existing structure for longer-term research. The current observational study could be pared down to a smaller cohort that is tracked to study how symptoms change into future decades, some experts suggested.
“I think this is an extraordinary cohort that cannot be replicated again,” Horwitz said of the observational study, pointing to the cohort’s size, diversity, and the extensive surveys and medical testing conducted on these participants. This testing is currently slated to end in two years, and “it’s of public health importance that we not throw that away” by providing additional funding, she said.
RECOVER’s pediatric research provides one example of a more successful part of the program that should receive continued support, said Megan Carmilani, a patient representative and founder of Long COVID Families. This research has identified how long COVID symptoms in children differ from adults and by age group, offering new information about this under-studied group of patients, she said. She has also found scientists leading this part of the program are more responsive to feedback from patient representatives like her than those leading the adult cohort, perhaps because this study started later, she said.
“There is no other study like RECOVER for pediatrics in the world,” Carmilani said. She would like to see RECOVER’s pediatric research gain additional funding to support clinical trials for children.
While keeping these valuable parts of RECOVER, many in the long COVID community would like to see the program become a “much leaner operation,” said Charlie McCone, a patient-advocate who has advised RECOVER. This would include paring down the adult observational study and the program’s extensive bureaucracy and focusing more on novel research, such as the types of studies Jain proposed.
According to advocates, the lion’s share of new federal funding should be directed to other offices and agencies focused more on biomedical innovation, supporting clinical trials, and improving medical care for people with long COVID.
One proposal, from PLRC and advocacy groups Long COVID Moonshot and Long COVID Campaign, calls for the federal government’s fiscal year 2025 budget to provide at least $1 billion to the NIH Office of the Director, so that funding can go to RECOVER as well as other programs; $200 million to Advanced Research Projects Agency for Health (ARPA-H), a newer agency that supports high-impact research; $20 million to the Office of Long COVID Research and Practice, which aims to coordinate long COVID work across the federal government; and $13.5 million to the Agency for Healthcare Research and Quality (AHRQ), to expand its support of best practices in long COVID medical care.
“We’d especially like to see the NIH Office of the Director fund a program of drug trials, developed in consultation with the patient community and clinicians and researchers with experience and understanding of studying long COVID in the context of [related diseases],” representatives from Long COVID Moonshot said in a statement.
The COVID-19 Longhauler Advocacy Project, a separate group, has similarly called for the fiscal year 2025 budget to support the NIH Office of the Director, the Office of Long COVID Research and Practice, and AHRQ, along with requesting funding for acute COVID-19 resources such as the Home Test to Treat program and wastewater surveillance. Other scientists and advocates suggest that the Department of Defense (DoD) and Biomedical Advanced Research and Development Authority (BARDA) may also be well-suited to funding meaningful long COVID research, due to their success with supporting COVID-19 vaccines as well as past funding for post-infectious disease research.
“DoD is phenomenal at running actionable, high-impact clinical trials fast,” Putrino said.
A different advocacy group, the Long COVID Action Project (LCAP), has requested $28 billion in funding based on analysis by health economist David Cutler. The group has proposed legislation that focuses on antiviral treatments, medical care, social supports, and COVID-19 prevention measures, modeled after prior HIV/AIDS laws, said LCAP founder Joshua Pribanic. All the health agencies “currently responsbile for the success of HIV/AIDS support,” a list that includes many of those also highlighted by other advocates, have a role to play in supporting people with long COVID, Pribanic said.
While advocacy requests from different groups vary in scale, all number in the billions as advocates explain that long COVID represents a national crisis with millions unable to work or do other day-to-day activities. “Failure to address this problem will result in significant economic, health, quality of life, and societal costs in the trillions of dollars,” advocates and scientists wrote in an open letter to President Biden last December, also calling for long COVID funding in the fiscal year 2025 budget.
McCorkell, from PLRC, said that her experience as a patient representative for RECOVER has often been just “trying to minimize harm.” She would like to see the program move to a position where patients are really helping to lead the research agenda, she added.
At a Senate hearing discussing the NIH’s fiscal year 2025 budget, agency director Monica Bertagnolli said people with long COVID and related diseases “have taught us over the last two years what we needed to do, now we just need to deliver for them.”
When asked to elaborate on those comments in an interview, Bertagnolli said that due to the work done over the last two years, with patient engagement and observational research, “we are now ready to do the studies that are designed… to be what those people who are suffering need to see.” Delivering for people with long COVID means “trials, trials, trials,” she added, while fundamental biology work will also continue.
RECOVER has an opportunity to demonstrate a renewed commitment to this patient community using the $515 million that it received earlier in 2024, McCone said. According to the NIH, these funds will be used for additional clinical trials and clinical research studies, extending observational research, managing RECOVER’s data and biospecimens, managing RECOVER’s data and biospecimens along with real-world data.
McCone summarized many patient-advocates’ message for RECOVER: “If you don’t like our criticism, if you think you can do things better, demonstrate it with the $500 million.”
Betsy Ladyzhets is an editor at The Sick Times. Her prior reporting on RECOVER, at STAT News and MuckRock in collaboration with Rachel Cohrs Zhang, was a finalist for the National Institute for Health Care Management Foundation’s journalism awards.
If you have tips to share with Betsy about RECOVER or other federal Long Covid programs, reach out to her at betsy@thesicktimes.org.
*Editor’s note: The Patient-Led Research Collaborative, like The Sick Times, has received support from the Balvi and Kanro funds. Our newsroom operates independently of financial supporters.
***
This article was published by The Sick Times, a new website chronicling the long COVID crisis, on May 31, 2024. It is republished with permission.






1 Comment
1 Comment